Palliative care is often unappreciated and underutilized in the care of persons with dementia. This disconnect can lead to increased suffering among patients, families, and caregivers. By applying a palliative approach to dementia care, nursing can significantly impact the quality of life – and death - among this growing population of patients.
Palliative care is the active, interdisciplinary care of patients with serious, advanced disease and their families. It emphasizes quality of life through multidimensional symptom management and family support. Expert communication assists patients and families in identifying goals of care and aligns medical treatments with those goals. (National Consensus Project, 2018). Furthermore, it is important to note that palliative care differs from hospice: palliative is offered at all stages of an illness trajectory, while hospice is geared toward the last six months of life. Palliative care is offered by teams of specialists with advanced training in the field; however, workforce limitations and an increasing geriatric population mandates that all levels of clinicians should be able to provide primary palliative care: basic symptom management, support, and communication (Wheeler, 2016).
Why is palliative care particularly helpful in dementia?
- Dementia is usually a long, progressive disease, which advances slowly over many years. This makes prognostication difficult, and disease progression is not always obvious to those closest to the patient. However, approximately one-third of people over 65 will die with dementia as a main or concurrent diagnosis (Eisenmann et al., 2021). Palliative care assists with advance care planning and brings an understanding of hospice eligibility criteria to bridge appropriate patients to hospice for the most appropriate care.
- Palliative care fosters a pro-active approach to care. Although decline may be slowly progressive, predictable symptoms and functional disability can be anticipated and proactively addressed. Preparation and advance planning for symptoms, nutritional issues, behavioral changes, and caregiver support can prevent a crisis-oriented, reactive trajectory, which leads to emotional and physical distress.
- While there is no cure for dementia, a comfort-oriented approach to care can be incorporated at all levels of illness. This involves non-verbal assessments of patients who lose the ability to communicate their needs and a proactive approach to pain and depression, feeding and toileting issues, and balancing stimulation with rest.
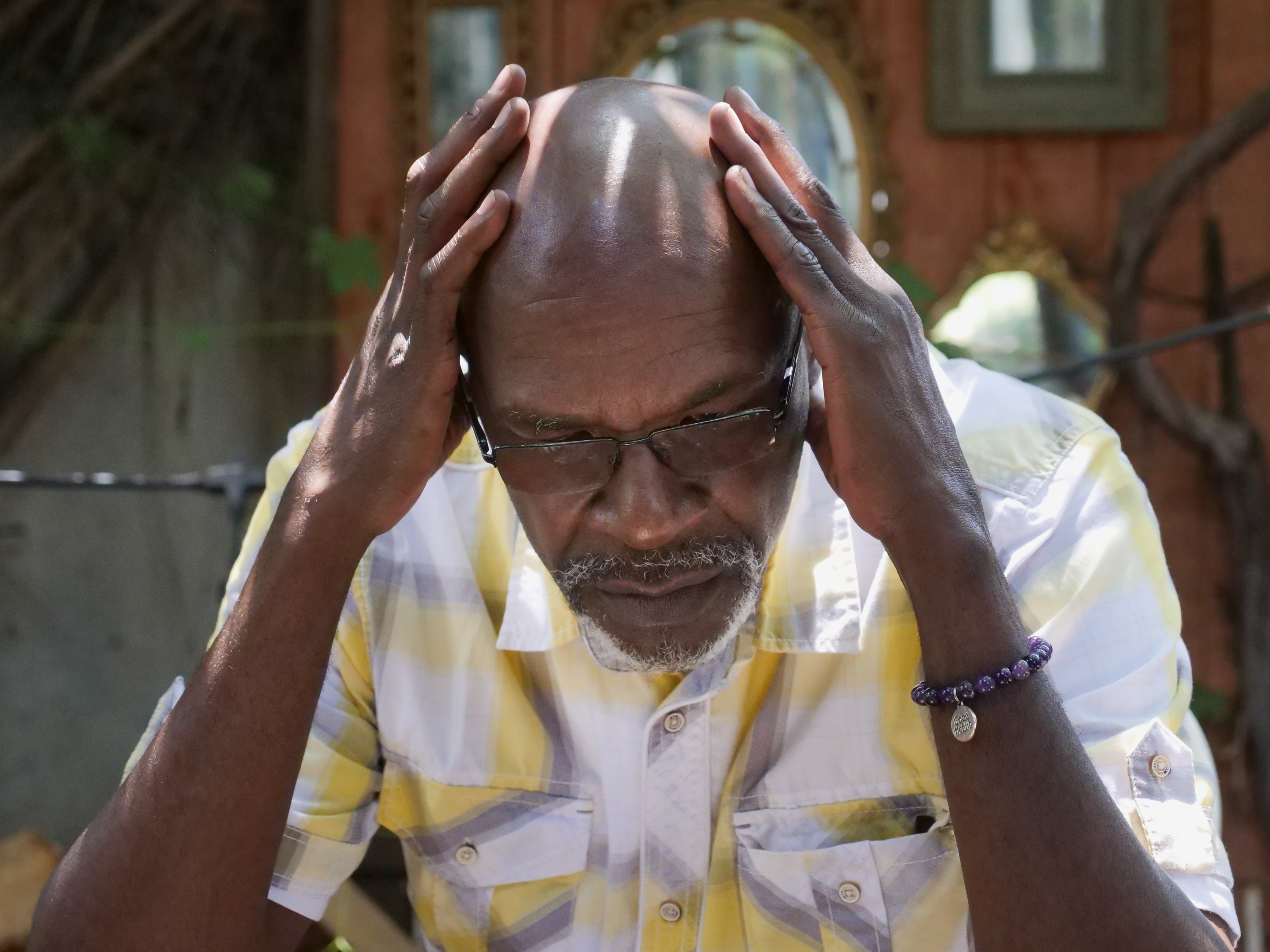
- Patients with dementia suffer from a myriad of specific dementia-related symptoms, which change as the disease progresses. Depression, delirium, dysphagia, immobility, pain, and neuropsychiatric symptoms can all develop along the path. Early recognition and a comfort-oriented approach can positively impact patients, families, and caregivers.
- With palliative care, the family is considered the unit of care. Family support is one of the basic pillars of care. A comfort-focused approach can assist families in moving from grief and helplessness to taking an active role in working with staff to find ways to provide active comfort. (Wyatt, 2019)
- Late-stage dementia accounts for about 40% of the total disease duration for the typical patient with Alzheimer’s disease. These patients often require institutional care with limited access to palliative care. Weight loss, feeding disorders, infections, and functional decline in dementia are indicators of poor prognosis (Mehta, 2021). Still, unfortunately, these issues often result in inappropriate and unhelpful hospital admissions and medical interventions. Palliative care approaches keep the big picture goals in the forefront of care and align medical treatment with those goals.
Dementia touches millions of patients and families each year, and the incidence will steadily increase as our population continues to age. Nurses who incorporate primary palliative care into their geriatric practice focus on symptom management, family support, and care planning that aligns care with patient goals. Keeping a comfort orientation can greatly impact the quality of life for this vulnerable population.
References
Eisenmann, Y., Golla, H., Schmidt, H., Voltz, R., & Perrar, K.M. (2021). Palliative care in advanced dementia. Frontiers in Psychiatry 11(10), 1- 15.
Mehta, Z., Giorgini, K., Ellison, N., & Roth, ME. (2021). Integrating palliative care with dementia care. Today’s Geriatric Medicine. https://www.todaysgeriatricmedicine.com/archive/031912p18.shtml
National Consensus Project for Quality Palliative Care. (2018). Clinical Practice Guidelines for Quality Palliative Care, 4th edition. Richmond, VA: National Coalition for Hospice and Palliative Care. https://www.nationalcoalitionhpc.org/ncp/
Wheeler, M.S. (2016). Primary palliative care for every nurse practitioner. JNP: The Journal for Nurse Practitioners, 12(10), 647-653.
Wyatt, A. (2019). Looking at palliative care through a dementia lens. Center to Advance Palliative Care. https://www.capc.org/blog/palliative-pulse-palliative-pulse-june-2017-looking-palliative-care-dementia-lens/

 Donation
Donation